Dr. Eitan Lerner is a molecular biophysicist at the Alexander Silberman Institute of Life Sciences. In biology, the structure of most proteins is related to their function. However, there is a group of proteins, intrinsically disordered proteins (IDPs), that are partially or sometimes even completely disordered or unstructured. These proteins can fold, bind, and function in many ways. In ordinary times, Dr. Lerner is studying how one such IDP, α-Synuclein, can on one hand support and facilitate proper dopamine release in our brains, but, on the other hand, can cause neurotoxicity associated with Parkinson's disease.
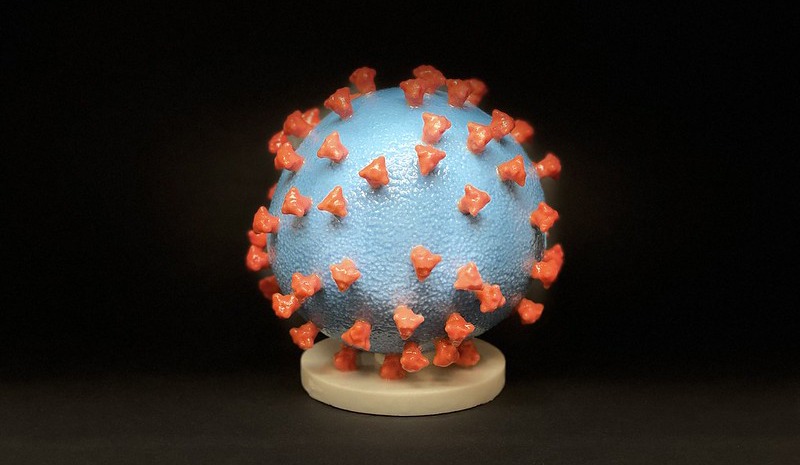
However, these are certainly not ordinary times. Following the outbreak of the COVID-19 pandemic, Dr. Lerner realized he had an opportunity to research something he had always been curious about: rapid counting of particles sized 50-500 nanometers, using light – a grey zone in biology, as most light-based observations focus either on much smaller biomolecular systems or much larger organisms. (The Coronavirus measures 100-120 nanometers in diameter).
A Different Method, Quicker Results
Dr. Lerner wondered if single-particle spectroscopy might be applied to developing a quicker Coronavirus diagnostic test. The standard PCR test takes 1-2 days to return results, leaving patients in limbo. Using single-particle spectroscopy, Dr. Lerner believed it would be possible to deliver equally accurate results more quickly. (See box for more info).
"We need an additional testing method, one that will complement the PCR-based testing, but that will provide faster results. Ideally, such a test would also be cheaper, saving the cost of reagents and other lab supplies."
Dr. Lerner got to work developing a microscopy-based apparatus for the counting of virus particles with high sensitivity and, most importantly, rapidly. He developed a method for detecting the presence of the virus based on two signatures: its size, determined by how many fluorescent molecules are displaced by the virus, and its specific interaction with proteins and antibodies – to confirm that the pathogen is, in fact, SARS-CoV-2 (and not a different particle of similar size). By confirming that the volume of displaced fluorescent liquid correlates closely with the observed antibodies – a viral detection event is recorded. The only thing that’s left is to count enough such events in a short period of time. The entire process can be completed in 10 minutes.
Looking forward, Dr. Lerner will begin testing the system with similar, safer viruses and antibodies supplied by various Hebrew University researchers, and eventually transfer his research to an existing BSL-2 lab.
Born Out of a Partnership
Dr. Lerner’s partner in this endeavor is Prof. Dr. Thorben Cordes at Ludwig Maximilian University (LMU) in Munich, who is responsible for the engineering aspects of the project. They already have the first prototype – a 3D-printed apparatus that uses readily available supplies. This would reduce costs, increase accessibility, and shorten wait-time – without compromising accuracy.
"We’ve refused to apply for grants requiring us to give up our intellectual property. If this method works, it must be immediately commercialized – for the benefit of humankind."
|
All diagnostic tests must balance specificity with sensitivity, while also providing results in a timely manner. Specificity refers to properly detecting the presence (or absence) of the pathogen, while sensitivity measures how much of the pathogen is needed to obtain a meaningful result. The Coronavirus is initially heavily present in saliva, as well as in other bodily fluids (to different degrees); as time passes and symptoms progress, the virus moves into host cells in the body – where it replicates and causes patients to transfer the virus to their surroundings. (Put on that mask!). A patient who is swabbed on the first or second day of their symptoms will have more virus in their saliva than a patient swabbed on the sixth or seventh day. Eventually, after approximately 14 days, so little virus will be found in these bodily fluids, that it may become harder to detect, forcing clinicians to rely on other methods (e.g. blood tests). Dr. Lerner has developed the technology that facilitates a test that is as specific and sensitive as the PCR test, but much quicker. It will complement the PCR test and perhaps come to serve as a rapid pre-test to help diagnostic teams in the field make better and quicker decisions, while helping patients get more accurate results - in less time. |
This research was supported by the ISRAEL SCIENCE FOUNDATION (grant No. 3565/20) within the KillCorona – Curbing Coronavirus Research Program
Photo credit: "Novel Coronavirus SARS-CoV-2" by NIH. Accessed on Flickr, used under a CC BY 2.0 license. The image has been cropped.


