The coronavirus is currently understood to enter the human body by interacting with a receptor named ACE2. This receptor is a protein that is displayed on the surface of certain cells in the lungs, nose, and oral cavity, among others. In a sense, the receptor and virus are like a keyhole and key; they must perfectly fit for the virus to enter and infect a person.
However, which cell types present ACE2 on their surface, and what determines their presence, is unknown. Prevent ACE2 from being displayed, or blocking its interaction with the virus, would likely reduce infection rates and stymie the virus’s ability to infect additional cells in the body. Furthermore, it is possible that the Coronavirus can enter the human body via additional gateway receptors, which could also potentially be targeted for therapy. Such other players are yet to be discovered.
It is clear that some recovered COVID-19 patients subsequently suffer from a range of illnesses, for example inflammation of the circulatory system in different organs. It is unclear whether the cells of these organs display gateway cells that permit infection by the virus.
Studying Healthy Cell Samples to Learn About Infection
Hebrew University scientists Dr. Oren Parnas and Dr. Yotam Drier, in collaboration with Hadassah lung surgeon Dr. Ori Wald, hope to provide answers to these questions. To this end, they are collecting cells from the lungs and other organs of non-COVID-19 patients. They are characterizing the exact gene activity profile of each cell and identifying which cell types display active ACE2 receptors. To date, they have profiled thousands of cells and measured the expression of hundreds of thousands of genes. Powerful computational tools are the only possible way to analyze such a vast dataset.
At the same time, the researchers are comparing their findings to existing cell databases to identify cell types with a proclivity towards SARS-Cov-2 infection. Their working hypothesis is that by identifying the type of cell, they will glean clues about the mechanism underlying COVID-19 symptoms. For example, inflammation of the circulatory system could be caused by direct infection of blood vessel cells.
"It may become possible to understand and treat the disease’s symptoms by understanding how it spreads in the human body – on a cellular level. This type of detective work can really allow us to trace the virus’s advancement within the body."
Dr. Oren Parnas
Looking Ahead: Uncovering a Gene Regulatory Network through Computer Analysis
Within our bodies, molecular networks regulate our genes, affecting when each gene is turned on and off. To fully understand how these networks are organized and how they work, Dr. Parnas and Dr. Drier will disrupt each of the known human genes in cells, one gene at a time, and then measure whether these perturbations change the cell’s ability to become infected with SARS-CoV-2.
It is possible that an eventual drug will target the regulatory mechanisms that enable infection, rather than combatting the virus at the site of infection. By creating a computational network of the genes’ regulatory mechanisms, scientists will be able to better understand – and disrupt – the chain of events that makes cells susceptible to infection.
The next step will be to translate these computational findings into lab experiments, in order to verify findings and determine the best course of treatment for patients.
"The impact of this groundbreaking work isn't limited to the current SARS-CoV-2 pandemic but will open the door to an entirely new understanding of how molecular networks affect disease and treatment - enabling us to treat numerous diseases more effectively."
Dr. Yotam Drier
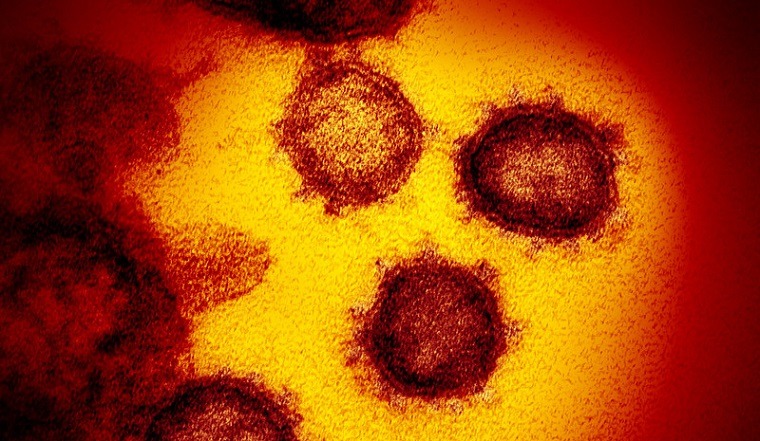
Photo credit: "Novel Coronavirus SARS-CoV-2" by NIAID. Accessed on Flickr, used under a CC BY 2.0 license. The image has been cropped.


